Larsson Rosenquist Foundation - Centre for Immunology and Breastfeeding
Our research
Why our centre?
Because improving child health requires closing the critical knowledge gap about their specific biological needs.
Children bear a disproportionate burden of disease, including infections, allergies, and malnutrition. Their physiological needs differ significantly from those of adults. They are in an incredibly dynamic phase of life, with the needs of their growing bodies evolving every day. For the very young, everything is new, and this is especially true for the immune system. It must learn to distinguish between what to fight, such as harmful pathogens, and what to tolerate, like their own microbiota or food. Yet most preventive and therapeutic strategies for infants are still modelled on adult systems.
We aim to transform early-life care by:
-
1. Raising awareness of the unique needs of the developing immune system, to support both short- and long-term disease prevention.
-
2. Bringing human milk into the equation
Human milk is a fluid that is far more than nutrition. It is rich in diverse compounds that complement and guide the child’s immune system. We view human milk as a dynamic reflection of the maternal–child environment, one that speaks the same biological language as the developing immune system.
-
3. Offering interventions that are truly aligned with their developmental needsToday, most treatments for newborns are the same as for adults, i.e. mainly the dose is modified. However, we are learning more every day about the differences between a newborn and an adult, and breast milk has known this for a long time. By studying the immunology of breastfeeding, our research has shown that human milk may know the best way to promote mucosal immunity in infants. We also seek to inspire the development of human milk-informed therapies tailored to infants’ specific developmental stage, improving lifelong health for all, from the very beginning. (Macchiaverni et al., 2024; van den Elsen et al., 2022)
-
4. Guiding mothers and health professionals to maximise the chances of disease prevention through breastfeeding
From pollutants to infection and dietary habits, the constituents of breast milk encapsulate a snapshot of the maternal environment, providing infants with a preview of the world they will inhabit. By investigating how human milk composition influences healthy immune development, we are paving the way for personalized advice that can help mothers maximise disease prevention through breastfeeding. Our research has suggested that consuming allergens while breastfeeding may be the best way to prevent allergies in children. Ongoing clinical trials led by our collaborator A/Prof Debbie Palmer should soon tell us whether this suggestion can become a recommendation.
-
5. Providing strong evidence to invest in breastfeeding support
Despite the World Health Organization's (WHO) guidelines promoting early initiation and exclusive breastfeeding, at least a third of newborns worldwide aren't benefiting from this optimal feeding practice, due to late initiation of breastfeeding or the administration of formula "supplements" that replace colostrum intake. We already know that colostrum is essential for reducing neonatal mortality in low resources settings. Our ongoing research will establish the importance of colostrum in preventing allergies, parasitic infections, stunted growth and much more.
Our research in a nutshell
A healthy immune system mounts efficient and well-regulated responses to protect us from a whole range of diseases, including infections, cancer, allergies, autoimmune conditions, gut inflammation, and malnutrition.
Our research aims to gain a deeper understanding of:
- How the child’s immune system operates
- What is required to lay the foundation for a healthy immune system
- Which factors shape immune development over time We place particular emphasis on breastmilk, a product of over a million years of evolution, as a dynamic, bioactive fluid that plays a key role in both establishing early immune foundations and guiding their development during this critical window of life.
-
1. Laying strong foundations for a healthy immune system
Our research focuses on a critical and underutilised opportunity for preventive health: the first days of life. By targeting this brief but transformative period, we aim to define interventions with the greatest long-term impact on child health.
The transition from fetus to newborn is the most complex adaptation in the human experience. The fetus leaves a sterile, aquatic environment—where physiology is deeply entwined with the mother’s—to suddenly breathe through the lungs, rely on external nutrition, and face exposure to billions of microbes.
At this crucial moment, the mother produces colostrum, the first milk, available during the first three days of life. Often called “liquid gold,” its composition appears uniquely tailored to support this transition. Yet, at least one in three newborns worldwide receives formula supplements during this period, as if colostrum alone were not sufficient.
While colostrum’s composition is well described, its specific long-term health benefits remain poorly documented, particularly outside of neonatal survival in low-resource settings. To fill this gap, we conduct preclinical and clinical research in birth cohorts from both low- and high-income countries to investigate whether exclusive colostrum feeding is essential to set infants on a healthy trajectory.

We specifically study the role of colostrum in preventing allergy, growth failure, obesity, helminth infection, neurodevelopment and skin diseases. This knowledge will support WHO guidelines implementation and drive the discovery of developmentally appropriate, colostrum-inspired strategies to prevent childhood diseases from the very first day of life.
-
2. Educating the immune system through breast milk
Some consider the infant immune system to be immunodeficient—for example, because infants do not yet produce antibodies at levels comparable to adults. However, this view overlooks the maternal–infant immunological dyad. A full-term newborn receives antibodies via the placenta and continues to receive mucosal antibodies through breast milk. This illustrates the inadequacy of studying the child’s immune system in isolation, without considering the mother's contribution.
Beyond complementing the infant’s immune system, breast milk plays an active role in educating it. It shapes the infant’s gut microbiota by contributing to its initial seeding and by providing selective nutrients that support beneficial microbial growth. Breast milk also contains environmental antigens—derived from allergens and pathogens present in the maternal–child environment. We are investigating how antigen shedding via breast milk helps train the infant’s immune system to mount appropriate future responses: promoting tolerance toward allergens and effective defense against pathogens. This immune education is further modulated by a range of bioactive compounds in breast milk whose composition is influenced by the mother’s physiology and environment. Altogether, this supports the broader concept that breast milk reflects the maternal exposome and prepares the infant for life in their specific environment.

By investigating how the maternal environment shapes milk composition and, in turn, immune development, we are laying the groundwork for personalised guidance to help mothers optimise disease prevention through breastfeeding.
By studying how breast milk shapes early immune responses, we are generating essential knowledge to inform the development of infant-tailored therapeutics, such as next-generation vaccines.
Transformative knowledge
-
1. Laying strong foundations is required for food allergy prevention
Using data from an Australian birth cohort (the ORIGINS cohort), we demonstrated that a child’s diet at birth significantly influences their risk of developing peanut and multiple allergies within the first year of life, with colostrum emerging as highly protective. Our findings further suggest that adequate colostrum feeding may reduce the need for strict early peanut introduction, broadening the strategies available for peanut allergy prevention (Bhasin et al, 2025). Until now, formula supplementation has mainly been considered in the context of cow’s milk allergy risk. With this publication, we aim to raise broader awareness of how early formula use may interfere with colostrum feeding, with potential consequences for multiple aspects of child health—well beyond cow’s milk allergy.
Our research opens new perspectives for peanut allergy prevention, including the promotion of colostrum feeding and the development of colostrum-inspired therapeutics for infants at risk, who require formula for medical reasons or whose mothers are unwilling to breastfeed.
-
2. Educating the immune system through breast milk
Our research challenged the allergen avoidance paradigm by demonstrating that egg allergens in maternal milk can educate the infant immune system toward immune tolerance, thereby reducing the risk of allergy (Verhasselt et al., 2008 (Verhasselt et al., 2020). We further uncovered why breast milk is more effective at promoting immune tolerance than direct allergen exposure: allergens in breast milk are present in very low amounts, and the presence of bioactive compounds such as cytokines, antibodies, and vitamins—all shaped by maternal physiology and the maternal exposome—modulates the efficacy of tolerance induction (Adel-Patient et al., 2020; Mosconi et al., 2010)(Rekima et al., 2017) Turfkuyer et. al, 2016). Our work contributed to the 2014 food allergy prevention guidelines, which were updated in 2020 (Halken et. al., 2021 Murano et al., 2014) and was summarised in our recent review emphasising the need to consider the infant’s immune requirements and maternal input through breast milk when designing targeted prevention strategies (Macchiaverni et al., 2021; Verhasselt 2024). In collaboration with an expert in dietary prevention of allergy, Debbie Palmer and the ORIGINS cohort, the LRF-CIBF continues to explore how to maximize the potential for allergy prevention through maternal intervention and breastfeeding, including researching the benefits of incorporating dietary recommendations for mothers—such as increased fibres intake (Divakara et.al., 2024).
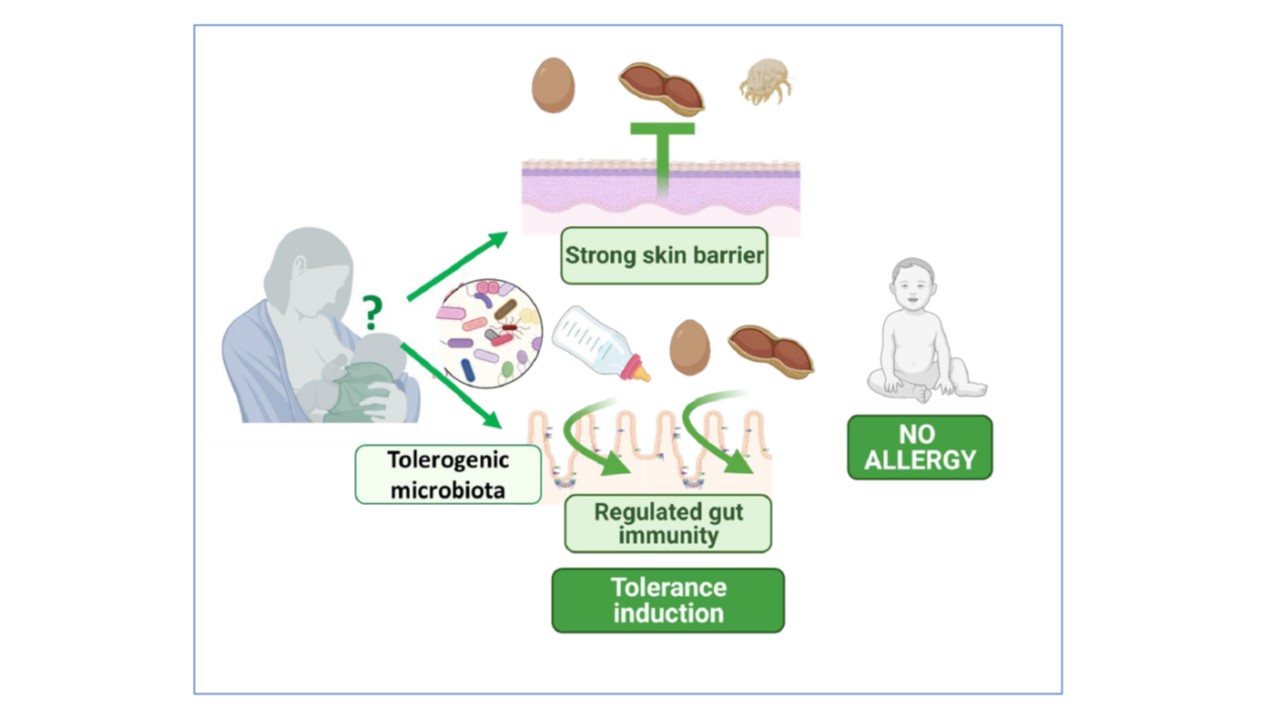

Our findings support the broader concept that breast milk reflects the maternal exposome and is exquisitely suited to prepare the infant for life in their specific environment. This opens the door to targeted maternal recommendations during breastfeeding, aiming to optimise the early-life window for allergy prevention.
-
3. Unlocking the potential of colostrum
Helminth infection: In a unique preclinical model of colostrum deprivation, we demonstrated that colostrum is essential for the expansion of key immune cells in the gut—type 2 innate lymphoid cells (ILC2s)—which are critical for controlling helminth infections Rekima et al (2024).. In a proof-of-concept birth cohort in Uganda, we further found that providing newborns with the first drops of colostrum was associated with a significant reduction in helminth infections during childhood (Rekima et al., 2024). Globally, more than 1.5 billion people—approximately 25% of the world’s population—are infected with soil-transmitted helminths. Infected children often suffer from nutritional deficiencies, stunted growth, and impaired cognitive and physical development, with profound societal and economic consequences.

Stunting: Using the same preclinical model, we found that age-inappropriate feeding—specifically providing mature milk instead of colostrum at birth—leads to chronic inflammation and growth failure, despite mature milk being higher in energy and produced in larger volumesVan den Elsen et al . These findings strongly suggest that the primary role of colostrum in the first three days of life is not nutritional in the conventional sense, but rather to lay the foundation for regulated energy metabolism and healthy growth. Chronic undernutrition affects 200 million children and leads to irreversible developmental disorders such as growth failure, immune dysfunction and neurodevelopmental deficits, or death in 3 million children each year.

Our research has also shown that the diet in the first days of life plays a critical role in food allergy prevention. Ongoing studies suggest it may be equally important for supporting healthy skin development and preventing neurodevelopmental delays.
This research provides new evidence for an overlooked yet scalable solution to reduce major global disease burdens in both high- and low-resource settings, including malnutrition, helminth infections, and allergies: promoting colostrum feeding. It also paves the way for a paradigm shift in newborn care and precision prevention, inspired by the biological compounds found in colostrum and their specific targets in the developing infant.
-
4. Pathogen antigen shedding in breast milk for optimal infant immune priming
Breastmilk is the most effective evidence-based strategy for preventing infectious diseases in early life, saving up to one million lives annually(Victora CG, 2016). One of its most powerful features is the real-time transfer of maternal antibodies against pathogens present in the shared maternal–child environment, representing one of the clearest examples of personalised medicine in nature Verhasselt 2024(Verhasselt et al., 2024). Building on our observations that certain antigens in maternal milk, such as house dust mite allergens, can stimulate long-term immune responses in offspring (Baiz et al., 2017; Macchiaverni et al., 2014; Rekima et al., 2020), we proposed that the transfer of microbial antigens via breast milk may have been evolutionarily selected to prime the infant immune system and actively promote protective immunity (Marchant et al., 2017; van den Elsen et al., 2022; Verhasselt, 2015). Pathogens or pathogen-derived antigens in breast milk could function as naturally attenuated vaccines or antigens accompanied by immune-modulatory compounds tailored to the infant’s developing mucosa (Marchant et al., 2017; van den Elsen et al., 2022; Verhasselt, 2015). We recently provided proof of concept for this hypothesis in the context of malaria, demonstrating that Plasmodium antigens are indeed present in human milk (van den Elsen, et al. 2022).

Learning from breast milk, whose most recognised effect is the prevention of infectious disease, will reveal the unique needs of the infant’s immune system for effective protection. It offers insights not only into reinforcing immune defences, but also into actively shaping immunity to pathogens for optimal long-term protection.
Our priorities in the next 5 years
- Target vulnerable populations
- Bring knowledge on the importance of breastfeeding in healthy skin development
- Promote allergy prevention through Breastfeeding
- Prioritize our partnerships with Asia
Meet our team
Prof Valerie Verhasselt
Director of the LRF-Centre for Immunology and Breastfeeding
My passion is to learn from Nature to find the best solutions to promote healthy immune development. With a background in Internal Medicine and more than 20 years of research in Immunology, I want to put the mother-child dialogue through breast milk at the heart of understanding how to reduce the burden of child disease in both high and low-income countries, including allergies, malaria, worm infections, and growth failure. I strongly value creativity and discovery research. Not having a specific goal allows you to be completely open, discover what you did not expect, and marvel at it. And it's in this sense of wonder and freedom of mind that the most beautiful ideas are born, ideas that, without meaning to, can change the world. Importantly, as a Team leader, it is a source of immense gratification to contribute to the empowerment of my team members, to make them aware of their huge potential and to see them blossom.
Further information
Dr Patricia Macchiaverni
Program Manager
I am a biologist with a background in Immunology and extensive experience in clinical and translational research in both academic and industrial settings. My academic journey began with a Bachelor's degree in Biological Sciences and Education, followed by a Ph.D. in Immunology. After completing my PhD in 2012, I worked for four years as a Senior Scientific Manager in multinational pharmaceutical companies, where I gained valuable expertise in project management, team leadership, and effective communication of scientific data to diverse audiences. In 2017 I joined the LRF-CIBF as a Research Fellow, investigating the link between breastfeeding and allergy prevention in children. Now, as a Programme Manager at LRF-CIBF, my goal is to promote global excellence, foster collaboration, and facilitate communication. I'm all about making science fun and impactful!
Savannah Machado
Research Assistant
As an enthusiastic research assistant at the LRF-CIBF, I have flourished in our dynamic environment. Beginning as a volunteer in 2019, I pursued a master's degree in Biomedical Science, and eventually transitioned into my current research assistant role. This journey has allowed me to delve deeper into exploring colostrum's role in food allergy prevention, with a current focus on the prevention of egg and peanut allergies, through pre-clinical models. Infant health and development have long been my primary research passions, driving my efforts to understand and promote early-life factors essential for optimal growth and disease prevention.
Professor Wayne Thomas
Honorary researcher
I am an emeritus professor at the University of Western Australia and an emeritus research fellow at the Kids Research Institute Australia. I previously served as a senior principal research fellow with the Australian National Health and Medical Research Council and earned my PhD from the University of Western Australia. Following that, I completed postdoctoral research at the Medical Research Council Clinical Research Centre in London and the Walter and Eliza Hall Institute in Melbourne. Since 1984, my research has focused on the immunology of allergy and infectious diseases in children, as well as experimental models, based in Perth at Princess Margaret Hospital for Children. I was also a founding member of what is now known as The Kids Research Institute Australia. I am widely recognized for my work in determining the structures and immune responses to house dust mite allergens and their epitopes. My broader research interests have spanned seminal cellular studies of cytokine production, immunological tolerance, experimental immunotherapy, and cat allergy. More recently, I have explored immune responses to viral and bacterial infections that precede the development of childhood asthma.
Further information
Students
Collaborators and funders
-
Global Human Milk Research Consortium (GHMRC)
Our team is proud to be one of the five independent research centres that make up the prestigious Global Human Milk Research Consortium (GHMRC). Working together, we are committed to advancing the frontiers of human milk and breastfeeding research on a global scale, making a meaningful contribution to the UN Sustainable Development Goals and WHO Global Targets.
-
The ORIGINS Project
The ORIGINS Project is the largest study of its kind in Australia, following 10,000 children, from their time in the womb, over a decade to improve child and adult health. Our Centre has two ongoing sub-projects using the ORIGINS cohort: the GAP study (Gateway for Allergy Prevention) and CEED study (Colostrum Exclusivity and Early Development).
-
Our main collaborators
- Public health - Pete Gething and Dr Susan Rumisha, Geospatial Health and Development team, TKI; Sofa Rahmania, PhD, UWA, Prof. Rosalind Gibson and Prof. Lisa Houghton, New Zealand.
- Pediatricians - including Prof. Suzan Prescott (School of Pediatrics and Child Health, University of Western Australia, Perth, Australia), Dr. Ravisha Srinivasjois ( Joondalup Health Campus) Prof. Desiree Silva (The Kids Research Institute Australia and Joondalup Health Campus);, Prof George du Toit (Kings College London, UK), Dr Stéphanie De Smet (Hopital de l’Archet, France)
- Dietician - experts in child nutrition and allergy prevention: A/Prof Carina Venter (University of Colorado, USA); Dr Debbie Palmer (The Kids Research Institute Australia, Perth, Australia); Dr Therese O Sullivan (Edith Cowan University, Perth)
- Lactation - consultants Louisa Connoly, president of Lactation college (Perth, Australia) ; Kirsten Tannenbaum, Australian Breastfeeding Association (Australia)
- Infectious disease - Dr. Thomas Egwang (Kampala, Uganda) project on colostrum and helminth/ breast milk and malaria; Dr Tim Barnett (The Kids Research Institute Australia, Perth, Australia), Nelly Amenyogbe and Prof. Tobias Kollmann (Dalhousie University, Canada) colostrum and sepsis; Rick Maizels, Glasgow University, helminth infection; A/Prof. Lea- Ann Kirkham ear health among Aboriginal children (TKI). Juan Rodriguez, Madrid University and Dr. Allison Imrie, UWA, Breast milk and COVID-19; Dr. Leshan Wannigama- Thailand.
- Neurodevelopment - Prof. Giancarlo Natalucci ( Zurich University)
- Health economics - Prof. David Yanagizawa-Drott (Zurich University)
- Biochemistry - Dr. Lars Bode (UCSD) and Dr. Fadil Hannan (Oxford)
- Microbiota - Prof. David Lynn, (SAMHRI); Dr. Claus Christopherson (Curtin University, Perth, Australia); Remy Burcelin, Inserm, France
- Transcriptomic analysis - Dr. Tom Iosidifis and Dr. Patricia Agudelo, The Kids Research Institute Australia
- Epigenetics - Dr. David Martino, The Kids Research Institute Australia
- Skin - Mark Fear UWA, Prof Fiona Wood, UWA, and Asha Bowen, The Kids Research Institute Australia Perth
-
Funders
CIBF is one of the five chairs endowed by the generous donation of the Family Larsson Rosenquist Foundation By providing financial independence in perpetuity, this endowment enables us to pursue panoramic research with long horizons, in complete independence and freedom of research and teaching.
We are also grateful to receive grant support from:
- Western Australia Child Research Foundation
- Future Health Research and Innovation Focus Grant
- Channel 7 Telethon Trust
- The Kids Research Institute Australia collaborative award
- Westfarmer Centre of vaccines and Infectious Disease (WCID) seed and partnership grant
- Open Philanthropy
Global network

A TEAM partnering with over 30 collaborators across the globe
We work in synergy with global leaders in immunology, paediatrics, nutrition, allergy, infectious diseases, neurodevelopment, and public health. As one of five independent research centres in the Larsson-Rosenquist Foundation Global Human Milk Research Consortium (GHMRC), we contribute to advancing the global understanding of breastfeeding and child health across disciplines—from neurodevelopment and biochemistry to endocrinology, economics, and behavioural science. Input from our Consumer Group plays a vital role in guiding our research, ensuring our work stays relevant, applicable, and impactful.
Signature strengths
Our centre takes a collaborative, multidisciplinary, translational approach to provide a holistic understanding of the impact of breastfeeding on infant immunity. Our key strengths are:
Our centre has developed unique experimental models to understand complex biological processes related to breastfeeding's influence on infant immune development. These models provide invaluable insights into the mechanisms underlying maternal milk's influence on immune development.
We possess a rare expertise in newborn immunology and specialize in the analysis of human milk , including allergens and immunomodulatory compounds. This expertise allows us to unravel the intricate interactions between breast milk components and the developing immune system.
We have access to multiple large-scale birth cohort data sets from both high and low incomes settings, enabling us to verify our findings from the preclinical model and to guide our future fundamental research
Based at The Kids Research Institute Australia and affiliated to The University of Western Australia, our center benefits from world-class facilities, an esteemed academic community, and opportunities to mentor future researchers in children’s health.
We owe much of our success to the generous financial support and strategic guidance of the Larsson Rosenquist Foundation.
Strategic pillars
Innovation:
- We challenge existing dogma to provide newborns with personalized strategies tailored to their developmental age.
Collaboration:
- We foster collaborative international, multidisciplinary, and translational research to make high-impact discoveries.
Communication:
- Through a combination of publication in prestigious journals, presentation to a wide audience, and strong consumer involvement, we ensure that our findings reach those who can implement them and benefit communities worldwide.
Our values
We embrace humanity through the values of respect, kindness, openness, and generosity.
We are committed to excellence, learning from the experiences of others, from our mistakes, and always striving to do better.
We value teamwork and interdisciplinary collaboration, ensuring that the wonders of serendipity in discovery research lead to effective solutions for all.

Publications
The centre in numbers (2017 - 2025)
Publications: 82 | Citations: 5,734 | h-index: 37
Excellence: 84% of publications are in the top 25% journals by CiteScore
Impact: 60% are in the top 25% most cited publications worldwide and 22% in the top 10%
International Collaboration: 80% are co-authored with researchers in other countries
150 oral presentations across local, national, and international conferences including Plenary speaker in Australia, Asia and Europe conferences
-
Infection
- Colostrum is required for the postnatal ontogeny of small intestine innate lymphoid type 2 cells and successful anti-helminth defences. Rekima A, van den Elsen L, Isnard C, Smyth DJ, Lynn MA, Yee T, Stevens NE, Machado S, Divakara N, Bhasin M, Tjiam MC, Rowel C, Servant F, Burcelin R, Locksley R, Maizels R, Lynn DJ, Egwang T, Verhasselt V. 2024. IF 14. Top 1% Journal: This publication shows for the very first time that the diet at birth, colostrum is critical for long term health, and particularly the prevention of helminth infection. A huge burden of disease affecting 25% of the population and leading to dramatic developmental issues in children.Malaria Antigen Shedding in the Breast Milk of Mothers from a Region With Endemic Malaria. van den Elsen LWJ, Verhasselt V, Egwang T. JAMA Pediatr. 2020. IF 26. Top 1% Journal: This study brings a novel concept of possible malaria prevention through the presence of malaria antigens in breastmilk.
- Per Os to Protection - targeting the oral route to enhance immune-mediated protection from disease of the human newborn. Verhasselt V, Marchant A, & Kollmann T. R. J Mol Biol 2024.
- Maternal immunisation: collaborating with mother nature. Marchant A, Sadarangani M, Garand M, Dauby N, Verhasselt V, et al. Lancet Infect Dis. 2017.
- The neonatal window of opportunity-early priming for life. Renz H, Adkins BD, Bartfeld S, Blumberg RS, Farber DL, Garssen J, Ghazal P, Hackam DJ, Marsland BJ, McCoy KD, Penders J, Prinz I, Verhasselt V, et al. J Allergy Clin Immunol. 2018.
- Microbial antigen in human milk: a natural vaccine? van den Elsen LWJ, Kollmann TR, Verhasselt V. Mucosal Immunol. 2022.
- Specific IgA, But Not IgG, in Human Milk From COVID-19-infected Mothers Neutralizes SARS-CoV-2. Macchiaverni P, Lloyd M, Masters L, Divakara N, Panta K, Imrie A, Sánchez-García L, Pellicer A, Rodriguez JM, Verhasselt V. Pediatr Infect Dis J. 2024.
- What goes up must come down: dynamics of type 1 interferon signaling across the lifespan. Hartnell L, Agudelo-Romero P, Montgomery ST, Ben-Othman R, Verhasselt V, Stick SM and Kollmann TR. Immunol. 2025IF 5.9 top quartile (Q1) for immunology journals
-
Allergy
- Preventing food allergy in infancy and childhood: Systematic review of randomised controlled trials. de Silva D, Halken S, Singh C, Muraro A, Angier E, Arasi S… Verhasselt V, et al. Pediatr Allergy Immunol. 2020. IF 7. Top 10% journal: This guideline precedes the establishment of EAACI guidelines on food allergy prevention.
- A role for early oral exposure to house dust mite allergens through breast milk in IgE-mediated food allergy susceptibility. Rekima A, Bonnart C, Macchiaverni P, Metcalfe J, Tulic MK, Halloin N, Rekima S, Genuneit J, Zanelli S, Medeiros S, Palmer DJ, Prescott S, Verhasselt V. J Allergy Clin Immunol. 2020. IF 14. Top 1% Journal: In this publication we propose a paradigm shift: the presence of respiratory allergen in breastmilk from house dust mites, may represent a risk factor for food allergy. We have identified the mechanisms in the mice, which provides new targets to tackle for allergy prevention in breastfed children. We have also shown preliminary evidence of these findings in a birth cohort. This publication has been selected to be presented as Editor Choice to be published in the Issue of May 2020.
- Ovalbumin in breastmilk is associated with a decreased risk of IgE-mediated egg allergy in children. Verhasselt V, Genuneit J, Metcalfe JR, Tulic MK, Rekima A, Palmer DJ, Prescott SL. Allergy. 2020. IF 14, top 1% journal: This work is the translation of a study Prof. Valerie Verhasselt published in Nature Medicine, which proposed a novel concept of allergy prevention through oral tolerance induction through breastfeeding using a preclinical model. Here, we demonstrate for the first to demonstrate that having egg antigen in breastmilk may decrease egg allergy risk in children. This is a major step towards the identification of factors contributing to allergy prevention through breastmilk.
- Maternal diet during breastfeeding: Could it influence food allergy risk in children? Macchiaverni P, Divakara N, Verhasselt V. Encyclopedia of Food Allergy. 2024.
- Long-term reduction in food allergy susceptibility in mice by combining breastfeeding-induced tolerance and TGF-beta-enriched formula after weaning. Rekima A, Macchiaverni P, Turfkruyer M, Holvoet S, Dupuis L, Baiz N, Annesi-Maesano I, Mercenier A, Nutten S, Verhasselt V. Clin Exp Allergy, 2017.
- Early oral exposure to house dust mite allergen through breast milk: A potential risk factor for allergic sensitization and respiratory allergies in children. Baiz N, Macchiaverni P, Tulic MK, Rekima A, Annesi-Maesano I, Verhasselt V, et al. J Allergy Clin Immunol, 2017.
- Oral Tolerance Induction to Newly Introduced Allergen is Favored by a Transforming Growth Factor-beta-Enriched Formula. Holvoet S, Perrot M, de Groot N, Prioult G, Mikogami T, Verhasselt V, Nutten S. Nutrients. 2019.
- Prevention of Allergy to a Major Cow's Milk Allergen by Breastfeeding in Mice Depends on Maternal Immune Status and Oral Exposure During Lactation. Adel-Patient K, Bernard H, Fenaille F, Hazebrouck S, Junot C, Verhasselt V. Front Immunol. 2020.
- Preventing immediate-onset food allergy in infants, children and adults: Systematic review protocol. de Silva D, Halken S, Singh C, Muraro A, Angier E, Arasi S… Verhasselt V, et al. Pediatr Allergy Immunol. 2020.
- House dust mites: Does a clean mattress mean Der p 1-free breastmilk? Macchiaverni P, Gehring U, Rekima A, Wijga AH, Verhasselt V. Pediatr Allergy Immunol. 2020.
- The role of allergen-specific IgE, IgG and IgA in allergic disease. Shamji MH, Valenta R, Jardetzky T, Verhasselt V, Durham SR, Wurtzen PA, et al. 2021.
- Allergen shedding in human milk: Could it be key for immune system education and allergy prevention? Macchiaverni P, Rekima A, van den Elsen L, Renz H, Verhasselt V. J Allergy Clin Immunol. 2021.
- EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Halken S, Muraro A, de Silva D, Khaleva E, Angier E, Arasi S… Verhasselt V, et al. Pediatr Allergy Immunol, 2021.
- The role of milk feeds and other dietary supplementary interventions in preventing allergic disease in infants: Fact or fiction? Vandenplas Y, Meyer R, Chouraqui JP, Dupont C, Fiocchi A, Salvatore S, Shamir R, Szajewska H, Thapar N, Venter C, Verhasselt V. Clin Nutr. 2021.
- House Dust Mite Exposure through Human Milk and Dust: What Matters for Child Allergy Risk? Macchiaverni P, Gehring U, Rekima A, Wijga AH, Verhasselt V. Nutrients. 2022.
- Food Proteins in Human Breast Milk and Probability of IgE-Mediated Allergic Reaction in Children During Breastfeeding: A Systematic Review. Gamirova A, Berbenyuk A, Levina D, Peshko D, Simpson MR, Azad MB, Järvinen KM, Brough HA, Genuneit J, Greenhawt M, Verhasselt V, et al. J Allergy Clin Immunol Pract. 2022.
- A newborn's perspective on immune responses to food. Verhasselt, V. Immunol Rev, 2024. IF 8.3 top quartile (Q1) for immunology journals
- Effect of maternal prebiotic supplementation on human milk immunological composition: Insights from the SYMBA study. Divakara, N. Dempsey Z, Saraswati C, Garssen J, Silva D, Keelan J, Christophersen C, Cooper M, Prescott S, Palmer D, Verhasselt V, Macchiaverni P. Pediatr Allergy Immunol, 2024. Top 50% (Allery and Immunology) and Top 10% (Pediatrics)- IF 4
- Colostrum as a Protective Factor Against Peanut Allergy: Evidence From a Birth Cohort. Bhasin M, Cooper M, Macchiaverni P, Joys RS, O'Sullivan TA, Keelan JA, Venter C, Palmer JD, Lowe AJ, Prescott SL, Silva D and Verhasselt V. 2025.Top 1%- IF 14
- A newborn's perspective on immune responses to food. Verhasselt, V. Immunol Rev, 2024. IF 8.3 top quartile (Q1) for immunology journals
- Effect of maternal prebiotic supplementation on human milk immunological composition: Insights from the SYMBA study.Divakara, N. Dempsey Z, Saraswati C, Garssen J, Silva D, Keelan J, Christophersen C, Cooper M, Prescott S, Palmer D, Verhasselt V, Macchiaverni P. Pediatr Allergy Immunol, 2024. Top 50% (Allery and Immunology) and Top 10% (Pediatrics)- IF 4
- Colostrum as a Protective Factor Against Peanut Allergy: Evidence From a Birth Cohort. Bhasin M, Cooper M, Macchiaverni P, Joys RS, O'Sullivan TA, Keelan JA, Venter C, Palmer JD, Lowe AJ, Prescott SL, Silva D and Verhasselt V. 2025.Top 1%- IF 14
- Preventing food allergy in infancy and childhood: Systematic review of randomised controlled trials. de Silva D, Halken S, Singh C, Muraro A, Angier E, Arasi S… Verhasselt V, et al. Pediatr Allergy Immunol. 2020. IF 7. Top 10% journal: This guideline precedes the establishment of EAACI guidelines on food allergy prevention.
-
Microbiota
- Shaping the Gut Microbiota by Breastfeeding: The Gateway to Allergy Prevention? van den Elsen LWJ, Garssen J, Burcelin R, Verhasselt V. Front Pediatr. 2019.
- Risk Factors for Gut Dysbiosis in Early Life. Parkin K, Christophersen CT, Verhasselt V, Cooper MN, Martino D. 2021.
- Metagenomic Characterisation of the Gut Microbiome and Effect of Complementary Feeding on Bifidobacterium spp. in Australian Infants. Parkin K, Palmer DJ, Verhasselt V, Amenyogbe N, Cooper MN, Christophersen CT, Prescott SL, Silva D, Martino D. 2024.
- The Gut‒Breast Axis: Programming Health for Life. Rodriguez JM, Fernandez L, Verhasselt V. Nutrients, 2021.
- Shaping the Gut Microbiota by Breastfeeding: The Gateway to Allergy Prevention? van den Elsen LWJ, Garssen J, Burcelin R, Verhasselt V. Front Pediatr. 2019.
-
Malnutrition
- Human Milk Drives the Intimate Interplay Between Gut Immunity and Adipose Tissue for Healthy Growth. van den Elsen LWJ, Verhasselt V. Front Immunol. 2021.
- Diet at birth is critical for healthy growth, independent of effects on the gut microbiota. van den Elsen L. J. W, Rekima A, Lynn M. A, Isnard C, Machado S, Divakara N, Patalwala D, Middleton A, Stevens N, Servant F, Burcelin R, Lynn D. J, Verhasselt V. 2024.
- Human Milk Drives the Intimate Interplay Between Gut Immunity and Adipose Tissue for Healthy Growth. van den Elsen LWJ, Verhasselt V. Front Immunol. 2021.
-
Milk composition
- Nutritional and Non-nutritional Composition of Human Milk Is Modulated by Maternal, Infant, and Methodological Factors. Samuel TM, Zhou Q, Giuffrida F, Munblit D, Verhasselt V, Thakkar SK. Front Nutr. 2020.
- Antibodies in breast milk: Pro-bodies designed for healthy newborn development. Verhasselt, V., et al., Immunol Rev, 2024.IF 8.3 top quartile (Q1) for immunology journals
Community news
Community Engagement
Are you passionate about infant health and breastfeeding?
The LRF Centre for Immunology and Breastfeeding is leading research into how we can promote a happy childhood with optimal growth, no allergies, and no infections. We want to learn from human milk to provide the most appropriate care for newborn.
If you want to be involved, we invite you to join our consumer group.
By becoming part of our Consumer Group, you will:
- Share experiences and insights to help guide our research.
- Provide cultural guidance to ensure our research is inclusive and relevant to a broad community
- Help communicate research findings to families and communities
What is involved?
- Participate in 2x presential or virtual meetings per year.
- Review grant applications and lay audience communications (e.g., social media).
You will be compensated with an honorarium for your contributions and time
How to Get Involved: To express your interest or learn more, please contact us at: [email protected]

Contact us
Join us
If you're as passionate about human milk and infant health research as we are, we'd be thrilled to have you on board. Email us if you want to explore available opportunities further.
Location
- The Kids Research Institute Australia
- Northern Entrance, Perth Children's Hospital
- 15 Hospital Ave, Nedlands WA 6009
Contact
- Prof Valerie Verhasselt
- Director of the LRF-Centre for Immunology and Breastfeeding
- Dr Patricia Macchiaverni
- Program Manager