
Transforming lives and improving health outcomes in rural communities
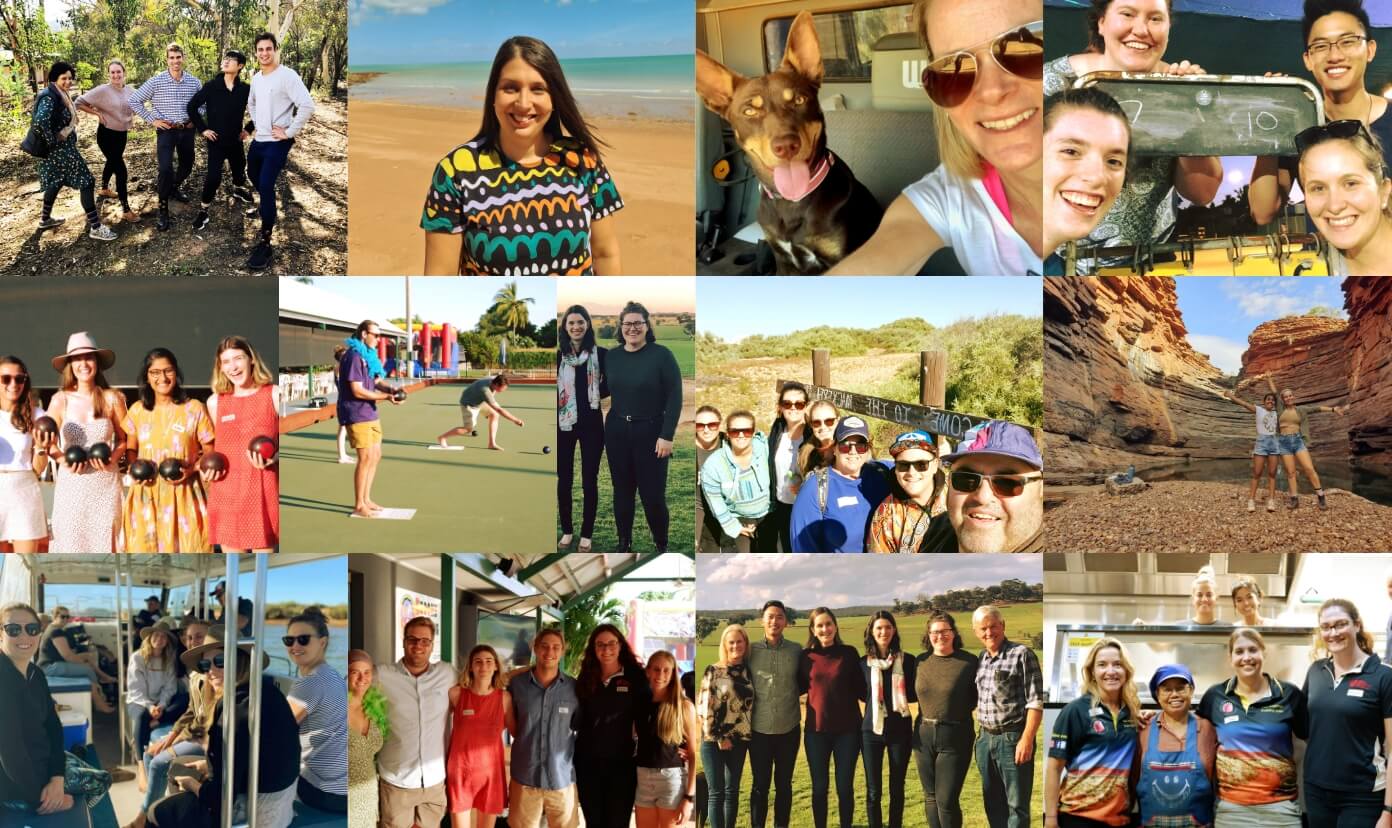
Collaboration is at our core
Acknowledgement of Country
We pay our respects to the Whadjuk Nyoongar Boodja Nation - the original lands of The University of Western Australia and The Rural Clinical School of Western Australia - which has now journeyed into many lands across the state. These are the lands that connect us and that we are now spiritually and physically bonded to, with the vision to help all who walk within The Rural Clinical School of Western Australia footprint. We acknowledge the strength, wisdom and courage of Whadjuk Nyoongar Boodja Nation Elders past, present and emerging.
We pay our respects to our neighbouring Nations, Tribes and visiting Peoples who share in the richness and uniqueness of our regions and who walk with us in our healing journey.
We acknowledge to all non-First Nation peoples who genuinely join us on our journey to ‘close the gap’ and abolish the disparities that exist.

Our Purpose
At the Rural Clinical School of Western Australia, we are passionate about teaching rural medicine, creating opportunities for students and medical professionals, and inspiring them to lead successful rural medical careers. While the challenges we face are great, we know our role is important and is making a difference in many communities.
Who we work with
Regional Training Hubs

We help shape your career in rural medicine
Be a part of real
community-driven impact
Join our team

Play a role in shaping the next generation of rural doctors
Follow their stories

The benefits you get from the RCSWA are the hands-on clinical experience, the exposure to things you would not otherwise see, and being really well supported in your learning.Dr Brittney Wicksteed
PGY3 Junior Doctor and RCSWA Broome Alumni, 2017

GP Management of Patient Depression and Suicidality
If you are a GP looking to enhance your skills in depression management and suicidality, then take advantage of this free online accredited learning and CPD opportunity.

Listen to Destination Medicine
With 81 fields of speciality practice including Rural Generalism to choose from, making a career decision can seem overwhelming for medical students and junior doctors. This podcast series sponsored by RCSWA Regional Training Hubs and featuring many of our alumni may help.

A legacy of service – Dr David Atkinson
The name David Atkinson is synonymous with rural medicine in Western Australia’s Kimberley and the Rural Clinical School of Western Australia, and it is not hard to see why.








